To better understand heart diseases, doctors and scientists are constantly trying to understand how cardiac tissue in the human heart is affected by its changing environment. Specifically, researchers have wanted to better understand how cardiac cells adjust themselves depending on the mechanical environment of the heart they are inside of. Some cardiac tissues adjust to the heterogeneous tissue mechanical environments, but studying this process is very difficult. Studying cardiac tissue inside a living person is extremely invasive and current cardiac tissue models outside the body often fail to demonstrate how cardiac cells adapt to the non-uniform changes.
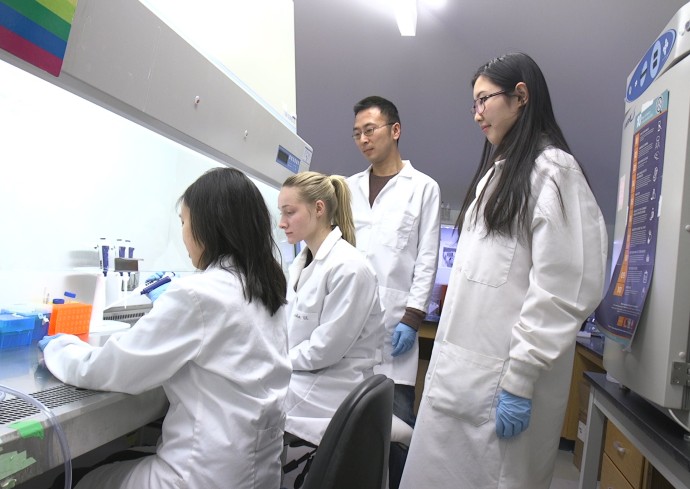
Zhen Ma, professor of biomedical and chemical engineering, and his research team—in conjunction with Professors Kevin E. Healy and Costas P. Grigoropoulos at the University of California, Berkeley—have developed a 3D cardiac microtissue model that allows for more realistic variations by cardiac cells. This research was recently published in the journal Advanced Healthcare Materials.
“We used engineering to mimic the mechanical environment of a diseased heart,” said biomedical and chemical engineering graduate student Chenyan Wang. Wang was the lead author on the published article.
The research team was able to use the cardiomyocyte cells derived from human stem cells to form 3D tissues on the biomaterial scaffolds made up of fibers with different mechanical properties. Ultra-fast lasers at the Berkeley Laser Thermal Laboratory were used to 3D-print these biomaterial scaffolds at high spatial resolution. The fibers with different mechanical properties allowed the researchers to see how heart tissue responded to non-uniform mechanical environments in a realistic way.
On video, the team was able to track the beating human cardiac tissues on the scaffolds in response to the mechanical changes and gather the quantitative data in a non-invasive way. Using human cells and 3D printing technology, Wang believes the 3D modeling can help advance the way we understand heart pathology with better, more realistic data.
“This could be a non-invasive method for analyzing cardiac behaviors and functions,” said Wang.
